Upper airway resistance syndrome 2018: non-hypoxic sleep-disordered breathing
William C. Arnold and Christian Guilleminault
Sleep Medicine, Stanford University, Redwood City, CA, USA
(The following contains a special report from the Expert Review of Respiratory Medicine 2019, VOL. 13, NO. 4, 317–326
https://doi.org/10.1080/17476348.2019.1575731)
Upper airway resistance syndrome (UARS) as obstructive sleep apnea syndrome (OSAS) has been described as abnormal breathing during sleep, based on the recording technologies and knowledge of the time. These terms have advanced the field, but are they still useful?
Historically, the definition of UARS syndrome was aimed at recognizing pathology not covered by ‘OSAS’ and to prompt specialists to go further than the obvious. It aimed at pushing specialists to recognize pathologies earlier and to elicit research in the developmental features of sleep disordered-breathing (SDB). The technology used to monitor SDB changed over-time, allowing recognition of SDB differently but not necessarily better.
For many years’ attention has been drawn only to ‘hypoxicsleep-disordered-breathing-H-SDB.’ This is related to the very prominent presence of obesity with co-morbid obstructive sleep apnea (OSA), and the easiness to use finger oximetry to diagnose patients.
Furthermore, it has led to many four channel-ambulatory recorders, with very limited investigation of ‘sleep-disordered breathing.’ Development of sophisticated equipment capable of treating any type of H-SDB, i.e. not only OSA but also REMsleep- related hypoventilation or hypoventilation syndromes, and the demonstration-particularly in the hypoventilation syndromes of the very successful outcome of decreases in hospitalization and improved quality of life, justify this effort. But, for many sleep disordered-breathing (SDB) began very early in life. We have indicated how problems may be suspected at birth and recognized even in early infancy. Specialists should now recognize and treat not Upper Airway Resistance
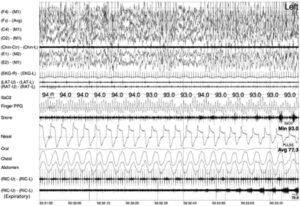
Syndrome ‘UARS’ but ‘non-hypoxic’ SDB avoiding further evolution of health problem and probable slow worsening overtime. Current sleep polysomnographic equipment, in laboratory or ambulatory, allows us to perform more sophisticated recordings than ever before- even if esophageal pressure probe (Pes) is still a gold standard- and allows us to perform appropriate analyses of recorded signals. The key issue is to monitor appropriately many variables and to know how to score them. The Brazilian group has defined on their population sample, the normative limits of ‘flow limitation’ in adults. Such investigation should be replicated, as nasal cannula allows appropriate recording of IFL, particularly when using a DC channel (see Figure 5). Appropriate investigation of the expiratory part of the breathing cycle may suggest the presence of abnormal airway resistance. Systematic analysis of mouth breathing during sleep should be mandatory, as mouth breathing always indicates an increase in airway resistance due to the tongue and mandibular position associated with mouth breathing supine, and any study of treatment should involve evaluation of appropriate nasal breathing during sleep, as restoration of normal nasal breathing is the only indication of successful treatment results.
Figure 5. Polysomnographic recording of a UARS patient. Channels from top to bottom: channels 1–4: EEG leads, channel 5: chin EMG channel 6 and 7: 2 eye movements channel, channel 8: ECG, channel 9 and 10: 2 leg EMG, channel 11: oximetry, channel 12: Finger-plethysmography, channel 13: snore volume, channel 14: nasal cannula, channel 15: oral channel (scoop), channel 16 and 17: Thoracic and abdominal inductive plethysmography bands, channel 18: intercostal/diaphragm muscles recording, channel 19: oblique – expiratory- muscle recording channel. As can be seen at beginning of recording segment nasal cannula already indicate flow limitation that get worse over time but is not associated with 3% SaO2 drop. Progressive snoring is recorded and increases in power with occurrence of increasing expiratory muscle activity. The arousal occurs just at the very end of the presented segment.
Currently, we have a better understanding of the development of SDB, and its evolution with aging, leading to co-morbid-OSA. However, the real issue is to recognize the problems much earlier, and to understand what can be done to prevent its development. The notions of OSA, UARS, apnea hypopnea index are only historical. There is enough knowledge to date to go beyond these definitions, to recognize problems differently and to lead to the prevention of the factors leading to SDB. The recognition of non-hypoxic sleep-disordered breathing is a step in this direction.
Read the full report here: